- EN - English
- CN - 中文
Plasma Membrane Wounding and Repair Assays for Eukaryotic Cells
真核细胞的等离子膜损伤和修复试验
发布: 2022年06月05日第12卷第11期 DOI: 10.21769/BioProtoc.4437 浏览次数: 3205
评审: Alka MehraAnonymous reviewer(s)

相关实验方案

新生儿心肺疾病的小鼠双击模型:支气管肺发育不良(BPD)和与BPD相关的肺动脉高压
Steven P. Garrick [...] Claudia A. Nold-Petry
2022年11月05日 4381 阅读
Abstract
Damage to the plasma membrane and loss of membrane integrity are detrimental to eukaryotic cells. It is, therefore, essential that cells possess an efficient membrane repair system to survive. However, the different cellular and molecular mechanisms behind plasma membrane repair have not been fully elucidated. Here, we present three complementary methods for plasma membrane wounding, and measurement of membrane repair and integrity. The first protocol is based on real time imaging of cell membrane repair kinetics in response to laser-induced injury. The second and third protocols are end point assays that provide a population-based measure of membrane integrity, after either mechanical injury by vortex mixing with glass beads, or by detergent-induced injury by digitonin in sublytic concentrations. The protocols can be applied to most adherent eukaryotic cells in culture, as well as cells in suspension.
Keywords: Cell injury (细胞损伤)Background
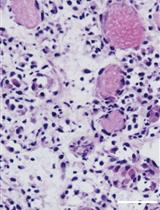
Unlike prokaryotic cells, which are protected by a cell wall, eukaryotic cells lack this shield, and are thus more vulnerable to membrane lesions (Cooper and McNeil, 2015). The plasma membrane of eukaryotic cells is composed of a phospholipid bilayer with integrated transmembrane proteins, which essentially constitutes the physical barrier separating the cell from the extracellular environment, and sustains an essential osmotic gradient to the outside (Khan et al., 2013). The integrity of the plasma membrane is frequently compromised during the lifetime of most cells by different means. Cells that reside in mechanically active tissue environments, e.g., muscle and lung cells, frequently experience injuries to their plasma membrane (McNeil and Khakee, 1992; Gajic et al., 2003). Both mechanical stresses and chemical stresses, such as pore-forming toxins secreted by invading pathogens (Bischofberger et al., 2009), can each induce membrane damage, which poses an immediate threat to cell survival if not repaired. Hence, cells have developed effective plasma membrane repair mechanisms to cope with membrane injuries and ensure cellular homeostasis. Repair mechanisms are strictly dependent on the influx of extracellular calcium ions (Ca2+) into the cell through the wound, and involve several cellular processes, including cytoskeleton reorganization (Abreu-Blanco et al., 2011b), exocytosis (Bi et al., 1995; Andrews et al., 2014), endocytosis (Idone et al., 2008), and membrane shedding (Scheffer et al., 2014; Jimenez et al., 2014; Sønder et al., 2019). The different repair mechanisms appear to be utilized in combination, depending on the kind of injury imposed on the membrane (Cooper and McNeil, 2015; Boye and Nylandsted, 2016). Furthermore, the influx of extracellular Ca2+ triggers rapid recruitment of various Ca2+-activated repair proteins to the damaged membrane, including members of the annexin family, which are directly involved in the immediate repair response, to seal the hole within seconds (A. K. McNeil et al., 2006; Bouter et al., 2011; Jaiswal et al., 2014; Boye et al., 2017; Sønder et al., 2019). The early repair responses occur within seconds to a few minutes after injury, and both the efficiency and underlying mechanisms of repair determine cellular fate: either cell death, or successful cell repair and restructuring. After initial membrane resealing, where annexins play a major role, cells need to restructure and remove damaged membrane, involving both exocytic and endocytic events, including macropinocytosis. To this end, we recently found that breast cancer cells use macropinocytosis coupled to components of the non-canonical autophagy system (a process termed LC3-associated macropinocytosis), to remove damaged parts of the plasma membrane, and restore membrane integrity (Sønder et al., 2021).
As loss of cell membrane integrity in vivo occurs due to a variety of physiological stressors, several experimental methods have been developed to mimic these conditions. These methods include cell-confined induced injury by passing cells through a narrow bore syringe, scraping attached cells from the substrate, or exposing cell monolayers to rolling glass beads (P. L. McNeil, 2001; P. L. McNeil et al., 2001; Corrotte et al., 2015; Jaiswal et al., 2014). However, these injury methods can be challenging to reproduce exactly, as they depend, for example, on the forces that are applied to the syringe, the cell confluency before scraping, or rolling with glass beads, resulting in great variability in the population of injured cells between samples. On the other hand, more controlled membrane lesions can be obtained using bacterial pore-forming toxins, e.g., Streptolysin O (SLO), which results in approximately 30 nm pores (Tweten, 2005; Idone et al., 2008). However, approaches using pore-forming toxins do not mimic mechanically-induced injuries in vivo, as these toxins chemically alter the cell membrane, by extracting lipids such as cholesterol (Gonzalez et al., 2008; Babiychuk et al., 2011). Thus, the choice of injury type is of great importance, since it can affect what can be learned about the repair response.
The first protocol presented here (Protocol A) is a method to monitor cell membrane repair kinetics in living cells, following UV ablation laser-induced plasma membrane injury. The two following protocols (Protocol B and Protocol C) are end point assays that can be used to identify, e.g., a deficit in the repair ability in different cellular conditions. Laser-induced injury is a very useful experimental approach, as it creates localized and well controlled injuries, which can be combined with live-cell imaging to follow fluorescently tagged proteins during the repair process (Jaiswal et al., 2014; Sønder et al., 2019). The laser injury approach has been used for monitoring cell membrane repair in various studies, in both mammalian and invertebrate organisms (McNeil et al., 2003; Abreu-Blanco et al., 2011a).
To analyze the extent of membrane damage and the kinetics of membrane repair, different fluorescent membrane impermeable dyes can be applied, including Hoechst 33258, propidium iodide (PI), FM1-43, and FM4-64. When the membrane is breached, Hoechst 33258 and PI, which are both membrane impermeant, can enter the cell and bind to nucleic acids. Here, the resulting fluorescence in the nuclei can be quantified as a measure of increased membrane permeability, i.e., poor membrane integrity. The FM dyes are styryl lipophilic dyes that increase in fluorescence intensity upon phospholipid binding. They will enter the cell through a membrane breach, thereby functioning as a read-out of the extent of injury and healing response, from which the repair kinetics can be calculated (Betz et al., 1996; Corrotte et al., 2015). However, FM dyes bind to the plasma membrane and are also taken up by the cell via endocytic mechanisms, which results in intense intracellular staining independent of membrane lesions over the long term. Thus, FM dyes are best suitable for measuring repair kinetics in short term assays. For long term assays, impermeable Hoechst 33258 or PI should be used instead, since these dyes only stain nucleic acids, and do not appear in internalized vesicles, as FM dyes do. For the laser-induced injury protocol, the cell membrane is injured by a high intensity single photon nanosecond pulsed laser, in presence of cell impermeant dye. The injury causes the impermeant dye to enter the cell, and repair restricts further dye entry, resulting in a fluorescence plateau. In contrast, failure to repair causes a continuous entry of the dye into the injured cell, and intracellular dye fluorescence will steadily increase.
The last two protocols presented here are end point assays, and provide a population-based measure for monitoring plasma membrane repair. End point assays are used to gain insight into the involvement of cellular and molecular processes in membrane repair. Their simplicity is an advantage when investigating novel repair proteins, and mechanisms involved in cellular repair, especially when investigating several conditions at the same time. However, the cellular repair response is a complex process that cannot be fully monitored without temporal resolution, which can be achieved using methods that enable controlled local injury of the cell membrane, and allow real time monitoring of the repair response. In both end point assays presented here, membrane integrity is measured using the membrane permeant dye Hoechst 33342, and membrane impermeant dye PI. By using a microscopy-based plate reader (Celigo® Imaging Cytometer), the number of total cells (Hoechst 33342 positive cells) and permeabilized cells (PI positive cells) are measured per well. An advantage of using image-based assays, to quantify membrane permeabilization and cell death, is that it provides information at the single cell level, as compared to enzymatic assays. In the first protocol, cells are mechanically injured by vortex mixing with glass beads (Protocol B), and in the second assay the cells are chemically injured using the detergent digitonin (Protocol C). Digitonin, a saponin from Digitalis purpurea (Sudji et al., 2015), is typically used in most laboratories to completely lyse cell membranes. However, it can also be used in sublytic concentrations, creating plasma membrane damage that can be repaired by cells (Boye et al., 2017; Heitmann et al., 2021). The exact mechanism of digitonin hole formation is still not clear, but known to be dependent on cholesterol in the membrane (Sudji et al., 2015). Therefore, the extent of membrane damage is dependent both on the cholesterol content in the plasma membrane, and digitonin concentration.
With these three protocols, we describe different plasma membrane wounding methods and membrane integrity assays. We have used these methods combined with siRNA knockdown of genes of interest, and pharmacological treatments [e.g., 5-(N-Ethyl-N-isopropyl) amiloride (EIPA), and trifluoperazine (TFP)], to elucidate the role of different repair proteins, including S100A11, and members of the annexin protein family, in membrane repair response to different types of injury (Jaiswal et al., 2014; Sønder et al., 2019; Boye et al., 2017; Heitmann et al., 2021; Sønder et al., 2021).
Protocol A: Plasma membrane repair kinetics upon laser injury in live cells
Materials and Reagents
RPMI 1640, without Phenol Red (Gibco® by Life Technologies, purchased via Thermo Fisher Scientific, catalog number: 32404014)
Trypsin, TrypLETM Express Enzyme (1×), no phenol red (Gibco® by Life Technologies, purchased via Thermo Fisher Scientific, catalog number: 12604013) (storage 4°C)
Fetal Bovine Serum (FBS) (Gibco® by Life Technologies, purchased via Thermo Fisher Scientific, catalog number: 10270106, 6%, storage 4°C)
GlutaMax (Gibco® by Life Technologies, purchased via Thermo Fisher Scientific, catalog number: 35050061, 2 mM, storage 4°C)
HEPES buffer solution stock 1 M (Sigma-Aldrich, catalog number: H3375, dissolved in H2O, storage 4°C)
Calcium-free imaging media (e.g., Hanks’ balanced salt solution (HBSS), without calcium, magnesium, nor phenol red (Gibco® by Life Technologies, purchased via Thermo Fisher Scientific, catalog number: 14175095, storage 4°C, use pre-heated to 37°C)
Cells tested in the current protocol
MCF7 human breast carcinoma cells
HeLa human cervix carcinoma cells
SH-SY5Y is a thrice-subcloned human cell line derived from the SK-N-SH neuroblastoma cell line
FM1-43 (Invitrogen, catalog number: T3163, 1.6 µM, store in aliquots -20°C)
FM4-64 (Invitrogen, catalog number: T13320, 2.5 µM, store in aliquots -20°C)
Propidium iodide (PI) (Sigma-Aldrich, catalog number: P4864, 0.5 µg/mL, stock 1 mg/mL, dissolved in H2O, storage 4°C)
Hoechst 33258 (Sigma-Aldrich, catalog number: 861405, 2.5 µg/mL, storage 4°C)
Cell imaging media (CIM) (see Recipes)
Equipment
Cell culture incubator set at 37°C, 5% CO2
35 mm, No. 1.0 Coverslip, 14 mm glass bottom, uncoated MatTek dish (MatTek Corporation, p35G-1.0-14-C)
Confocal microscope equipped with a spinning disk, ablation laser and a 63× water objective. In this protocol we use the following microscope and equipment:
Inverted microscope Eclipse Ti-E (Nikon) with a 63× water objective
UltraVIEW VoX Spinning Disk (PerkinElmer)
355 nm UV ablation laser (Rapp OptoElectronic)
Heated chamber (37°C) for live cell imaging
Software
Volocity software (PerkinElmers)
SysCon software (Rapp OptoElectronic)
Prism (GraphPad Software, Inc) or Microsoft Excel (Microsoft)
Procedure
文章信息
版权信息
© 2022 The Authors; exclusive licensee Bio-protocol LLC.
如何引用
Readers should cite both the Bio-protocol article and the original research article where this protocol was used:
- Sønder, S. L., Ebstrup, M. L., Dias, C., Heitmann, A. S. B. and Nylandsted, J. (2022). Plasma Membrane Wounding and Repair Assays for Eukaryotic Cells. Bio-protocol 12(11): e4437. DOI: 10.21769/BioProtoc.4437.
- Sønder, S. L., Häger, S. C., Heitmann, A. S. B., Frankel, L. B., Dias, C., Simonsen, A. C. and Nylandsted, J. (2021). Restructuring of the plasma membrane upon damage by LC3-associated macropinocytosis. Sci Adv 7(27): eabg1969
分类
癌症生物学 > 通用技术
细胞生物学 > 组织分析 > 损伤模型
您对这篇实验方法有问题吗?
在此处发布您的问题,我们将邀请本文作者来回答。同时,我们会将您的问题发布到Bio-protocol Exchange,以便寻求社区成员的帮助。
Share
Bluesky
X
Copy link