- EN - English
- CN - 中文
Expansion of Airway Basal Cells and Generation of Polarized Epithelium
气道基底细胞扩增和极化上皮细胞生成
发布: 2018年06月05日第8卷第11期 DOI: 10.21769/BioProtoc.2877 浏览次数: 14421
评审: Meenal SinhaAntoine de MorreeAnonymous reviewer(s)
Abstract
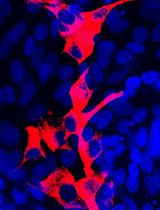
Airway basal stem cells are the progenitor cells within the airway that exhibit the capacity to self-renew and give rise to multiple types of differentiated airway epithelial cells. This stem cell-derived epithelium displays organized architecture with functional attributes of the airway mucosa. A protocol has been developed to culture and expand human airway basal stem cells while preserving their stem cell properties and capacity for subsequent mucociliary differentiation. This achievement presents a previously unrealized opportunity to maintain a durable supply of progenitor cells derived from healthy donors to differentiate into human primary airway epithelium for cellular and molecular-based studies. Further, basal stem cells can be harvested from patients with a specific airway disease, such as cystic fibrosis, enabling investigation of potentially altered behavior of disease-specific cells in the appropriate context of the airway mucosa. Here we describe, in detail, a protocol for the serial expansion of airway basal stem cells to enable the generation of nearly unlimited airway basal cells that can be stored and readily available for subsequent culturing and differentiation. In addition, we describe culturing and differentiation of airway basal stem cells on permeable transwell filters at air-liquid interface to create functional mucociliary pseudostratified polarized airway epithelial mucosa.
Keywords: Airway basal stem cells (气道基底干细胞)Background
Airway disease modeling and drug discovery have benefited greatly from the development and use of primary airway epithelial cultures grown on permeable transwell filters at air-liquid interface (ALI). This model has several advantages over immortalized cell lines in that the primary epithelial cells can differentiate into an airway mucosa that features multiple epithelial cell types including ciliated, serosal, and basal cells and their arrangement is quite reflective of in vivo cellular organization. Primary ALI models exhibit functional micro-physiological processes including beating cilia and the ability to secrete mucus, features which are notably absent in the cell line-derived epithelial monolayer. Further, primary cells do not rely on artificial immortalization or transformation, as cell line-derived epithelial cells do, and therefore are unencumbered by the potential deranged signaling seen in cell lines, which can misrepresent processes occurring in airway epithelium. Despite these notable limitations, immortalized cell lines are widely employed to model and investigate the airway epithelium because primary airway epithelial cells present their own set of challenges. Primary epithelial cells fail to replicate after a few passages and must be continuously harvested and isolated to complete each set of studies. In addition, molecular biology techniques to alter or delete the expression of genes of interest are difficult to achieve and sustain with primary epithelial cells. These disadvantages, creating both cost and technical hurdles, have hindered the widespread usage of primary ALI cultures despite their obvious advantages for investigating the airway mucosa.
Recently, transforming growth factor-β superfamily signaling (BMP/TGFβ/SMAD signaling) activity was found to be suppressed in p63+ basal cell compartments, but highly active in differentiated apically positioned cells (Mou et al., 2016). These observations facilitated the establishment of a novel culture platform with the use of dual SMAD inhibition to overcome the growth arrest and irreversible differentiation encountered in standard culturing of primary cells. Importantly, epithelial basal cell culture no longer relies upon co-culture of primary epithelial cells with mitotically inactive fibroblast feeder layers, a technique established in the 1970’s to enhance epithelial cell proliferation by improving the capacity of cultured cells to escape senescence (Rheinwald and Green, 1975). With this newly discovered ability to expand airway basal stem cells, patient-specific cells can be isolated and preserved from small biopsies of the airway, generating a virtually limitless supply of patient-specific airway epithelium in vitro (Mou et al., 2016). When differentiated on air-liquid interface, airway basal stem cell-derived epithelium forms a polarized mucociliary layer that exhibits proper epithelial architecture, physiology and response to clinically relevant pharmacologic agents (Mou et al., 2016; Yonker et al., 2017a and 2017b). Further, airway disease can be studied by generating basal stem cell-derived epithelium from individuals with airway disease, such as cystic fibrosis (CF), a genetic disease caused by a mutation in the CFTR gene, resulting in progressive respiratory failure. Primary ALI mucosa can be used to explore and understand cellular and molecular mechanisms that contribute to CF disease pathology.
Chronic infection and aberrant inflammation are hallmarks of CF (Yonker et al., 2015). Persistent infection with Pseudomonas aeruginosa, a typical pathogen in the CF airway, contributes to overzealous inflammation marked by pathological neutrophilic breach of the airway mucosa. A better understanding of cellular and molecular mechanisms mediating neutrophil trans-epithelial migration has the potential to inform and improve the efficacy of anti-inflammatory therapeutic strategies critically needed to treat inflammation mediated lung damage associated with CF. Recently, we have applied our advanced culture method in a co-culture system with neutrophils to investigate neutrophil-airway epithelium interaction and P. aeruginosa-induced neutrophil trans-epithelial migration (Yonker et al., 2017a and 2017b), Our findings from cultured human airway basal stem cells differentiated on ALI are consistent with prior molecular mechanistic studies implicating epithelial-derived neutrophil chemoattractant hepoxilin A3, an arachidonic acid metabolite synthesized by 12-lipoxygenase, as key in driving P. aeruginosa-induced trans-epithelial migration (Yonker et al., 2017a and 2017b). Additionally, these studies revealed previously unknown cellular mechanisms associated with neutrophilic breach of the airway mucosal barrier. Neutrophils applied to the basolateral aspect of the infected airway mucosal ALI organize in clusters before migrating through the mucosal barrier in response to epithelial infection. These organized clusters of neutrophils persist along the apical surface following trans-epithelial migration before individual neutrophils begin detaching from clusters into the airspace compartment (Yonker et al., 2017a). These results demonstrate that our expandable airway basal stem cell culturing and ALI differentiation system has tremendous potential to be exploited in a variety of ways to better understand micro-anatomy, physiology, interaction with pathogens, and innate immunity at the airway mucosa.
Below, we describe, in detail, a protocol for the generation of unlimited airway basal cells for the development of functional airway mucosal models that exhibit relevant physiological functioning. This protocol overcomes several barriers associated with investigations involving primary cells and represents a robust cellular platform for human disease modeling and drug development.
Materials and Reagents
- For airway basal cell expansion
- 6-well tissue culture plate (Corning, Falcon®, catalog number: 353046 )
- 150 mm tissue culture-treated culture dish (Corning, catalog number: 430599 )
- T175 culture flask (Thermo Fisher Scientific, catalog number: 159910 )
- 500 ml filter units (Merck, catalog number: SCGPU05RE )
- 804G cells
Note: 804G is a rat bladder epithelial cell line. It secretes matrix proteins enriched in laminin and collagen. The 804G-conditioned medium can be used as a cost-efficient coating medium. - Epithelial basal cell culture medium (Lonza, catalog number: CC-3118 or PromoCell, catalog number: C-21170 )
- Airway culture medium LHC-9 (Thermo Fisher Scientific, GibcoTM, catalog number: 12680013 )
- A8301 (antagonist of TGF/SMAD signaling, Tocris Bioscience, catalog number: 2939 )
- DMH-1 (antagonist of BMP4/SMAD signaling, Tocris Bioscience, catalog number: 4126 )
- CHIR99021 (agonist of WNT signaling, Tocris Bioscience, catalog number: 4423 )
- Y27632 (ROCK Inhibitor, Tocris Bioscience, catalog number: 1254 )
- Trypsin (Thermo Fisher Scientific, GibcoTM, catalog number: 25200056 )
- Penicillin-Streptomycin (Thermo Fisher Scientific, GibcoTM, catalog number: 15140122 )
- Dulbecco's phosphate-buffered saline (Thermo Fisher Scientific, GibcoTM, catalog number: 14190144 )
- RPMI 1640 medium, GlutaMAXTM supplement (Thermo Fisher Scientific, GibcoTM, catalog number: 61870036 )
- Fetal bovine serum (Thermo Fisher Scientific, GibcoTM, catalog number: 16000-044 )
- Complete Airway Basal Cell Culturing Medium (see Recipes)
- 6-well tissue culture plate (Corning, Falcon®, catalog number: 353046 )
- For airway-liquid-interface differentiation
- 0.22 μm filter (EMD Millipore, catalog number: SLGP033RS )
- 6.5 mm2 Transwell® with 0.4 µm Pore Polyester Membrane Insert, Sterile (Corning, catalog number: 3470 ), packaged 12 inserts in a 24-well plate
- 12 mm2 Transwell® with 0.4 µm Pore Polyester Membrane Insert, Sterile (Corning, catalog number: 3460 ), packaged 12 inserts in a 12-well plate
- PneumaCultTM-ALI Medium (STEMCELL Technologies, catalog number: 05001 )
- Hydrocortisone (STEMCELL Technologies, catalog number: 07904 )
- Heparin solution (STEMCELL Technologies, catalog number: 07980 )
- Sodium chloride (Thermo Fisher Scientific, InvitrogenTM, catalog number: AM9759 )
- 100% ethanol (Sigma-Aldrich, catalog number: E7023 )
- Complete ALI Medium (see Recipes)
- Hydrocortisone Solution (see Recipes)
- 0.22 μm filter (EMD Millipore, catalog number: SLGP033RS )
- For immunofluorescence
- Slides Thermofrost (Fisher Scientific, FisherbrandTM, catalog number: 12-550-15 )
- FisherbrandTM Cover Glasses: Rectangles (Fisher Scientific, FisherbrandTM, catalog number: 12-544-E )
- 2 ml Eppendorf tubes (Eppendorf, catalog number: 022431048 )
- ImmEdge Hydrophobic Barrier PAP Pen (Vector Laboratories, catalog number: H-4000 )
- Fluoromount-G (SouthernBiotech, catalog number: 0100-01 )
- DAPI (4',6-diamidino-2-phenylindole) (Thermo Fisher Scientific, Thermo ScientificTM, catalog number: 62247 )
- Triton X-100 (Sigma-Aldrich, catalog number: X100-500ML )
- 4% paraformaldehyde (Santa Cruz Biotechnology, catalog number: sc-281692 )
- Bovine serum albumin (Sigma-Aldrich, catalog number: A2153-100G )
- Sucrose (Sigma-Aldrich, catalog number: S7903 )
- OCT compound (Fisher Scientific, catalog number: 23730571 )
- Primary and secondary antibodies (see Table 1 below)
Table 1. Primary and Secondary antibodies for immunofluorescenceCatalog Number Vendor Name Target Primary antibody ab76013 Abcam Rabbit monoclonal, anti-NKX2.1, 1:200
Reacts with: Mouse, Rat, HumanAirway epithelium Primary antibody ab23630 Abcam Rabbit polyclonal, anti-FOXA2, 1:200
Reacts with: Mouse, Rat, HumanAirway epithelium Primary antibody ab53121 Abcam Rabbit polyclonal, anti-Cytokeratin 5, 1:500-1:1,000
Reacts with: Mouse, Rat, HumanBasal cells Primary antibody GTX102425 GeneTex Rabbit polyclonal, anti-p63, 1:300
Reacts with: Mouse, Rat, HumanBasal cells Primary antibody T6793 Sigma-Aldrich Mouse monoclonal (clone 6-11B-1), anti-Acetylated tubulin, 1:2,000-5,000
Reacts with: plant, pig, human, monkey, hamster, invertebrates, chicken, bovine, rat, frog, protista, mouseCiliated cells Primary antibody 14-9965-82 Thermo Fisher Scientific Mouse monoclonal (clone 2A5), anti-FOXJ1, 1:100
Reacts with: Mouse, HumanCiliated cells Primary antibody HPA031828 Sigma-Aldrich Rabbit polyclonal, anti-SCGB1A1 (CCSP), 1:200
Reacts with: HumanClub cells Primary antibody MA5-12178 Thermo Fisher Scientific Mouse monoclonal (clone 45M1), anti-Mucin 5AC antibody, 1:200-500
Reacts with: HumanGoblet cells Secondary antibody A-21202 ; A-21203 ; A-31571 Thermo Fisher Scientific Donkey anti-Mouse IgG (H+L), Alexa Fluor® 488, 594, 647 donkey anti-mouse IgG (H+L), 1:200 Mouse primary Ab Secondary antibody A-21206 ; A-21207 ; A-31573 Thermo Fisher Scientific Donkey anti-Mouse IgG (H+L), Alexa Fluor® 488, 594, 647 donkey anti-rabbit IgG (H+L), 1:200 Rabbit primary Ab Secondary antibody A-11055 ; A-11058 ; A-21447 Thermo Fisher Scientific Donkey anti-Mouse IgG (H+L), Alexa Fluor® 488, 594, 647 donkey anti-goat IgG (H+L), 1:200 Goat primary Ab
Equipment
- 250 ml bottles (Corning, PYREX®, catalog number: 1395-250 )
- Incubator at 37 °C with 5% CO2 (CO2 water jacketed incubator, Thermo Fisher Scientific, Thermo ScientificTM, catalog number: 3111 )
- Pipettes (PIPETMAN L Starter Kit, Gilson, catalog number: F167350 )
- Centrifuge with swing bucket rotor for 15 ml and 50 ml centrifuge tubes (Beckman Coulter, model: CS-6 )
- Vacuum pump
- Sterile laminar flow hood (The Baker Company, Sterilgard II )
- Hemostat or tweezers
- Scalpel
- 37 °C water bath (VWR, catalog number: 89501-468 )
- 4 °C cold room
- Inverted Light microscope (Nikon, diaphot TMD)
- Olympus Fluoview FV10i confocal microscope
- Olympus IX81 inverted fluorescence microscope (Olympus, model: IX81 )
Software
- ImageJ software (downloaded from https://imagej.nih.gov/ij/)
Procedure
文章信息
版权信息
© 2018 The Authors; exclusive licensee Bio-protocol LLC.
如何引用
Levardon, H., Yonker, L. M., Hurley, B. P. and Mou, H. (2018). Expansion of Airway Basal Cells and Generation of Polarized Epithelium. Bio-protocol 8(11): e2877. DOI: 10.21769/BioProtoc.2877.
分类
干细胞 > 成体干细胞 > 上皮干细胞
细胞生物学 > 细胞分离和培养 > 细胞生长
细胞生物学 > 细胞分离和培养 > 细胞分化
您对这篇实验方法有问题吗?
在此处发布您的问题,我们将邀请本文作者来回答。同时,我们会将您的问题发布到Bio-protocol Exchange,以便寻求社区成员的帮助。
Share
Bluesky
X
Copy link